A 55-year-old woman in rural Rwanda presents to the hospital with progressively worsening dyspnea and lower extremity and abdominal swelling. She cooks daily using an indoor stove with harvested wood.
This case will guide you through a clinical encounter to understand the patient's health challenges – and how to respond.
LEARNING OBJECTIVES
Identify local and global environmental factors that contribute to air pollution
Describe the human health effects of indoor and outdoor air pollution and associated health inequities
Recognize air pollution as a threat to planetary health
CLINICAL COMPETENCIES
Perform a detailed (and locally adapted) environmental history to identify environmental hazards that relate to patient’s presentation
Recognize sentinel cases of potential air-pollution-related health effects
Demonstrate the use of an environmental hazard risk assessment framework to guide clinical decision making
Demonstrate how to obtain, interpret, and utilize data on air quality to impact patient care
Create preventive treatment plans that include improvement of host vulnerability (host factors) and reduction of environmental exposures to air pollution
A Continuing Medical Education activity presented by the Stanford Center for Innovation in Global Health and the University of Washington. View CE information and claim credit HERE.
Accreditation
In support of improving patient care, Stanford Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation
American Medical Association (AMA)
Stanford Medicine designates this Enduring Material for a maximum of 1.5 AMA PRA Category 1 Credits™.
Physicians should claim only the credit commensurate with the extent of their participation in the activity.
American Nurses Credentialing Center (ANCC)
Stanford Medicine designates this Enduring Material for a maximum of 1.5 ANCC contact hours.
American Academy of Physician Associates (AAPA)
Stanford Medicine has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria.
This enduring activity is designated for 1.5 AAPA Category 1 CME credits. Approval is valid until December 14th, 2026. PAs should only claim credit commensurate with the extent of their participation.

Approach to Air Pollution Exposure
Consider the following as you work through this case:
Assess the patient:
Recognize signs of air pollution exposure
How susceptible / vulnerable is the patient? (host factors)
Assess the environment:
How much air pollution?
What other environmental risks for air pollution?
Manage the patient:
Treatment of the disease that is affected by air pollution
Improvement of other host factors
Reduce exposures / improve the environment:
Reduce exposure to air pollution
Reduce air pollution
History
Taking a clinical history of your patient yields the following information:
Chief complaint
History of present illness
Past medical & surgical history
Medications
Allergies
Family history
Social & environmental history ("Social-E")
Review of systems
Discussion
What else would you want to know?
What parts of the physical exam would you pay closer attention to?
Key Points
Learn how to do assess the health risks of an environmental hazard (in this case air pollution):
Step 1: Hazard identification (what could a patient be exposed to?)
Step 2: Exposure assessment (how much exposure?)
Step 3: Risk characterization and assessment (given the hazard and degree of exposure, how much risk is there to the patient?)
Step 4: Assess for patient host factors that enhance patient’s susceptibility to this exposure risk
Step 5: Clinical management and prevention:
Treat acute disease
Improve host factors (e.g., treat underlying conditions)
Improve environmental factors (e.g., reduce exposure, reduce pollution)
Exposure to indoor air pollution:
Follow-Up Questions for Patient
Asking your patient the following questions gives you this information:
What is your home made of? Floors and roofing?
What fuel do you cook with? To heat your home?
Is your kitchen indoors or outdoors? In a shared or separate room?
Are there windows or a chimney for ventilation?
Do you burn candles or other objects indoors?
Do you have indoor pets? Are they sick?
Exposure to outdoor air pollution:
Do you live in a large city, town, or rural area?
Are you aware of any pollution sources near your home?
Do you perform physical activity outside?
What sort of work do you do? Do you notice any dust or other hazards at work?
Do you spend time near heavy traffic?
What form of transportation do you use?
Are there fires or dust storms near you?

Discussion
What parts of the physical exam would you pay closer attention to?
Physical Exam
When you examine your patient, you learn the following:
General
Head Eyes Ears Nose Throat (HEENT)
Neck
Chest & lungs
Cardiovascular
Abdominal
Genitourinary
Skin
Lymphatic
Musculoskeletal
Neurologic
Discussion
What is your differential diagnosis?
Based on the clinical context, is there any additional testing you would pursue?

Diagnostics & Other Testing
information that will be helpful in diagnosing your patient:
Labs: White blood cell count 4000 cells/mm3 (eosinophil count 300), hemoglobin 13.6 g/dL, normal aminotransferases, total bilirubin 3 mg/dL, creatinine 1.2 mg/dl
Rapid HIV test: Negative
Sputum for geneXpert molecular TB test: Negative
Kato-Katz (looking for helminths such as Schistosomiasis in the stool): Negative x2
Electrocardiogram (ECG): Sinus tachycardia at 110, right axis deviation, an incomplete right bundle branch block pattern, right atrial enlargement
Imaging – chest radiograph: Prominent right cardiac border, flattened diaphragms, scattered increased interstitial markings
Transthoracic echocardiogram: Moderate-severe right ventricular hypertrophy, right ventricle and right atrium were moderate-severely dilated. Mild left ventricular concentric hypertrophy present with ejection fraction 65%. The valves were structurally normal, but there was moderate tricuspid regurgitation with right ventricular systolic pressure calculated at 45 mm Hg, using an estimated right atrial pressure of 20 mm Hg.
Differential Diagnosis
based on what you’ve learned so far, here’s how you might think about a differential diagnosis:
Pulmonary
Cardiac
Infectious
Gastrointestinal
Renal
Discussion
How could air pollution exposure be related to the differential diagnosis?

Pulmonary hypertension and cor pulmonale with probable COPD
Pulmonary function tests and CT radiography were not available. History, exam, and echo findings are consistent with right heart failure (RHF), and based on history, exam, and x-ray it was presumed that she has COPD.
Rates of isolated/concomitant RHF appear to be higher in LMICs, including those in sub-Saharan Africa.
The most common causes of RHF are thought to be: HIV, schistosomiasis, and lung parenchymal destruction from TB, COPD, and other diseases.
Final Diagnosis
arriving at a conclusion:
Indoor air pollution
Contact with and (suspected) exposure to air pollution ICD-10 code Z77.
Indoor air pollution is associated with increased development and exacerbations of COPD, as well as mortality among women. It is hypothesized that indoor air pollution may be a risk modifier for pulmonary hypertension and RHF beyond the association with COPD, but more research is needed.

Management & Treatment
approaches to helping your patient:
Patient was given IV furosemide while admitted and switched to oral furosemide.
She was treated with albuterol nebulizers and then given albuterol and long-acting anticholinergic inhalers for home.
Home supplemental oxygen was not available, and she was weaned off oxygen with SpO2 >92% in room air.
Prevention
You can reduce patient vulnerability and environmental exposures through the following considerations:
Reducing exposures / improving environments (environmental factors)
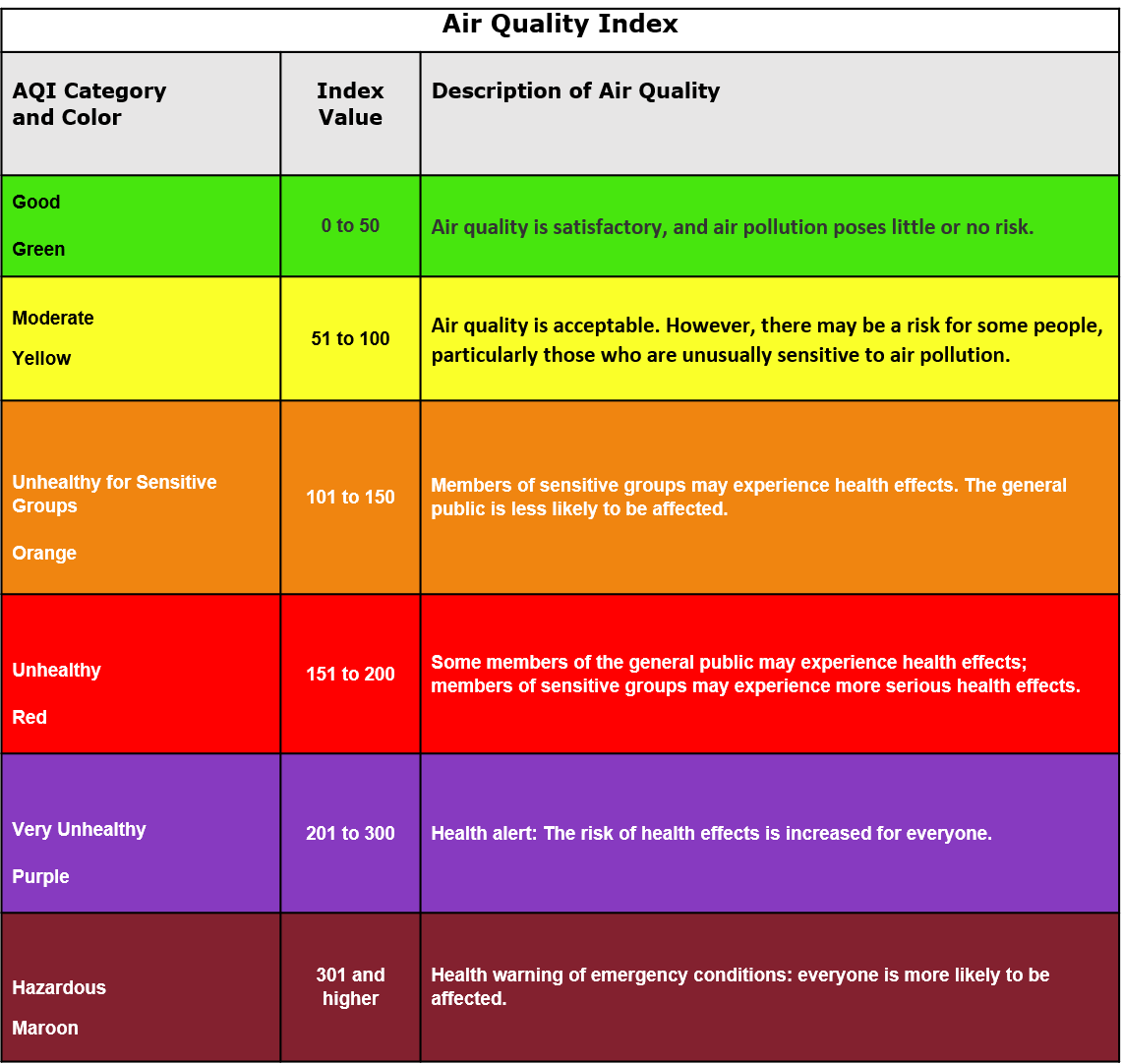
Treating environmental factors involves assessing sources of air pollution both outdoors and indoors and taking steps to reduce exposure – which could involve assessing outdoor exposure through air quality index (AQI) if available and/or asking the patient whether symptoms worsen in certain environments (e.g., indoors).
Consider wearing a mask around exposure to dusts.
If feasible, consider indoor air purifier.
If cooking contributes to indoor air pollution, steps to reduce exposure include switching to cleaner fuels, partitioning a kitchen space, relocating cooking to outside, or adding a chimney or window near the stove.
When outdoor air pollution gets to dangerous levels, staying indoors as much as possible (if the indoor environment is safer) and wearing masks if outside are key steps to preventing negative health impacts.
Consider other vulnerable household members, particularly young children in the case of cookstove-related smoke exposure.
To prevent even more air pollution-related health problems, brainstorm ways to reduce outdoor air pollution. For example, a change in transportation from using a motorbike to walking or biking if local air quality allows, will not only help your patients breathe cleaner air but also their entire community – others outside of your patient’s household may be vulnerable to air pollution as well. Avoid trash burning. Reduce agricultural burning.
Reducing host vulnerability / susceptibility (host factors)
Treating host factors involves optimal treatment of heart failure and COPD.
Assessing for changes in lung function over time, nutritional status, and food insecurity.
Smoking cessation if applicable.
Long-term healthcare maintenance and vaccinations.
Access to inhalers if applicable.

Beyond the Clinic
Local and global factors contribute to indoor and outdoor air pollution.
The home is a key source of indoor air pollution in many settings, especially in low- and middle-income countries (LMICs). Understanding common sources of indoor pollution can help pinpoint the source of the patient’s symptoms.
Many sources of indoor pollution are local in nature, such as combustion products, chemicals, radon, and biological products. Combustion products are responsible for the majority of indoor air pollution in LMICs, as in this case.
Most outdoor air pollution of concern is created by humans – such as through traffic pollution or industrial pollution – or exacerbated by humans via climate change, such as smoke from wildfires and dust particulate matter from worsening droughts. The health effects of individual pollutants are difficult to isolate, as they are usually mixed together in our atmosphere. Regardless, no amount of outdoor air pollution is “safe” for humans.
Direct sunlight and warmer temperatures from climate change result in an increase in ground-level ozone formation, which has been linked to asthma and COPD. Furthermore, the combination of extreme heat and air pollution exacerbate the health effects of each other, leading to a vicious cycle.
Increased NO₂ levels can also reduce the biodiversity of plant communities, and ozone damages tree leaves. Imbalanced ecosystems can change disease dynamics and forest fires cycles, and agricultural crop yields decrease when exposed to pollutants.
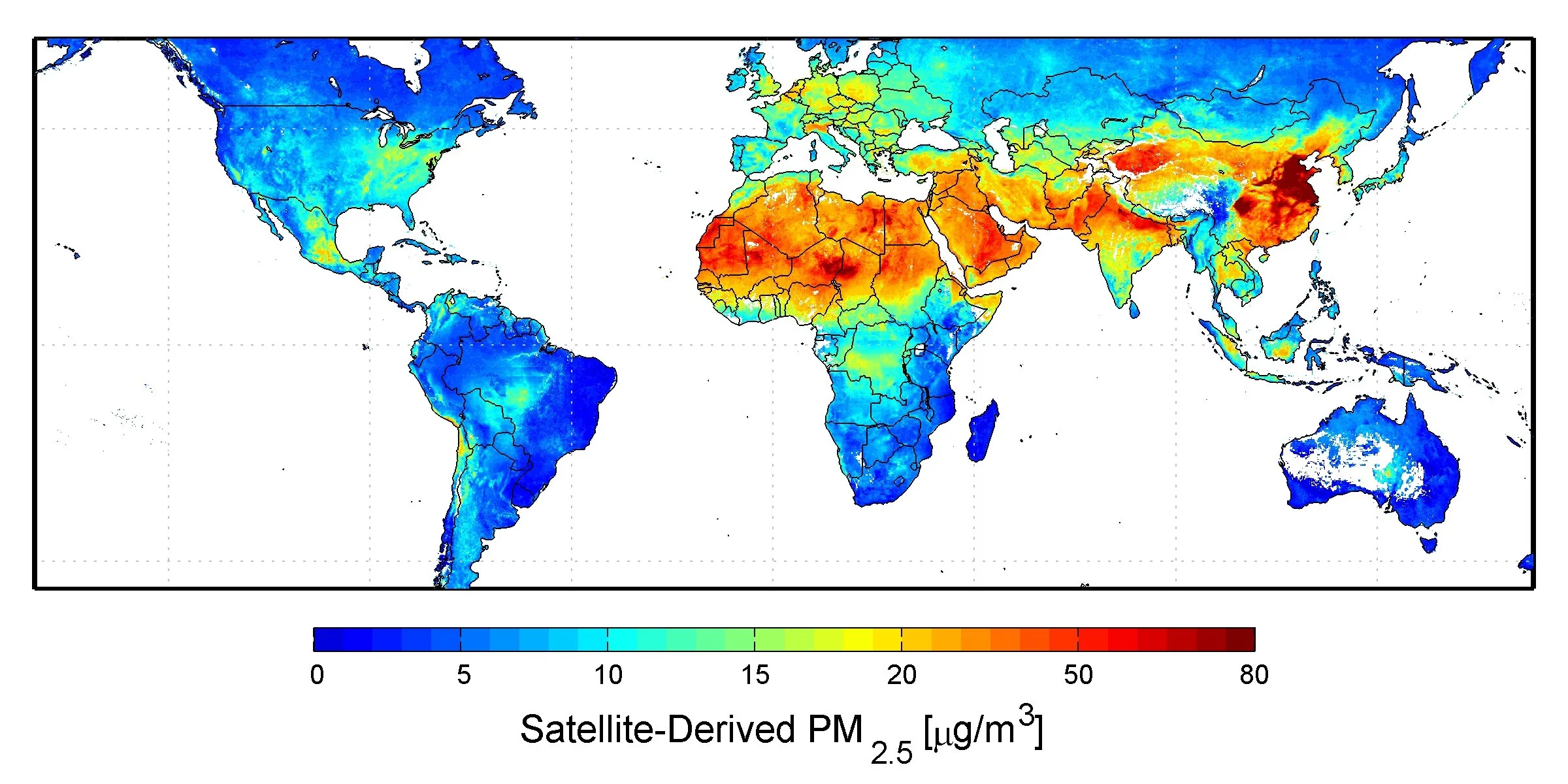
One useful tool to gauge the level of outdoor air pollution is the AQI (air quality index), which signifies current pollutant levels, including ozone, PM10, and PM2.5. It uses a normalized scale from 0 to 500: the higher the AQI value, the greater the level of pollution. An AQI is generally based on national air quality standards, so index values can differ by countries. However, many areas of the world, particularly in Africa, lack any air quality data. AQI standards are also based on ambient air pollution, not accounting for potentially far more toxic pollutants and volatile chemicals, such as those found in wildfire smoke.
Percentage of 2019 DALYs attributable to air pollution (DALYs are disability-adjusted life-years). From Figure 6 of Lancet 2020; 396: 1223–4.
Air pollution’s impacts are not equally felt across different socioeconomic classes and countries. Certain groups are more susceptible to the health consequences from air pollution – and may not be able to easily avoid air pollution in their environments. Health professionals should develop skills to diagnose the impacts of air pollution and devise treatment plans that take into account unique patient life circumstances.
Patients in LMICs suffer from more health consequences due to air pollution (see map below). Within both higher- and lower-income countries, socioeconomic status also can determine individuals’ exposure to sources of pollution; lower-income jobs might require working outdoors in polluted air or in facilities with indoor pollutants and poor ventilation, and industrial zones are more likely to be next to low-income neighborhoods.
In terms of indoor pollution, around 3 billion people cook using open fires or simple stoves fueled by kerosene, biomass, and coal, mostly in LMICs. Each year, 3.8 million people die prematurely from illness attributable to indoor air pollution. In homes with limited ventilation, household exposure to particulate matter may be 100 times higher than WHO standards, and in these dwellings, women and young children are most highly exposed.
In terms of outdoor air pollution, 91% of the world population lives in places where the WHO air quality guidelines levels are not met, and 98% of cities in LMICs with more than 100,000 inhabitants do not meet WHO air quality guidelines. Outdoor air pollution was estimated to have caused 4.2 million premature deaths in 2016, with 91% of those deaths in LMICs.
AQI Table, US EPA
SOURCES OF PARTICULATE MATTER AIR POLLUTION FROM FACTS.NET
Case Follow Up
What happens next:
The patient improves and is discharged home. She is able to receive an improved biomass cookstove from a local nonprofit agency. Over the next month, she is able to gradually increase her activity level.

Call to Action
Clinicians can take action to advance planetary health:
At the clinic:
Talk to your patients about risks from wildfire smoke, pollution from vehicle exhaust and industrial activities, recreational and occupational exposures, and indoor cooking.
Where it’s financially and logistically possible, encourage the switch from gas to electric induction stovetops. Natural gas stoves have been shown to release methane, a greenhouse gas 25 times more potent than carbon dioxide, and harmful pollutants, such as carbon monoxide. In the United States, the Inflation Reduction Act will provide rebates for low-income families making the switch to electric. In lower resource settings worldwide, there are a number of improved biomass cookstoves that use less fuel and emit less smoke. Even better, solar-powered electric cooking may become a cheap, eco-friendly option in the near future.
In your community:
Report increased number of cases to health authorities.
Join efforts to improve air filters in public settings, such as schools, and homes. This can go a long way in curtailing the effect of air pollution, especially in wildfire events.
Support local decarbonization efforts by joining a local citizens’ climate group or attending town hall meetings related to climate change to express your valued perspective. By switching to renewable energy that emits much less pollutants into the atmosphere, your community will enjoy cleaner air and better health for everyone.
Find out if there are any intervention or prevention studies available. If so, consider enrolling the patient.
At the societal level:
Advocate for clean energy by meeting with lawmakers at all levels of governance (local, state, national) and writing op-eds on this issue. Renewable energy reduces industrial pollution, which is disproportionately concentrated in lower-income communities, and combats climate change, which contributes to other sources of air pollution through wildfires and drought.
Pay attention to local legislation and support effective policies and policy makers.
Summary and
Key Learning Points
Also available for download here:
Air pollution, both indoor and outdoor, can adversely affect respiratory and cardiac function in patients. Prolonged exposure to air pollution can cause COPD and lead to right heart failure.
Vulnerability to air pollution (host risk factors):
Underlying cardiac disease
Underlying lung disease
Older age
Infants
Respiratory infection
Exposure risks (environmental risk factors):
Indoor cookstoves
Poor ventilation
Animals in house
Wildfires and other fires nearby
Dust storms
Outdoor air pollution from energy use and transportation
Pollen
Screening questions for the Social-E part of the patient history:
Are your symptoms worse in particular environments or with particular activities?
Is there an indoor cookstove?
Are you aware of fires or other outdoor sources of air pollution?
Based on screening questions, follow-up questions about exposures include:
Type of stove
Type of fuel for cooking and heating
Ventilation in house
Awareness of outdoor air pollution
Proximity to traffic areas or other sources
Visible haze indoor or outdoor
Assessing risk to patient:
What is the exposure?
How much exposure? (look for data sources on air pollution; example)
How much risk? (from 1 and 2)
How vulnerable is the patient?
Combined assessment of risk based on 3 and 4
Preventive management:
Reduce host vulnerability (improve risk factors: optimize cardiac and respiratory status)
Reduce exposures: change cookstove/fuel type, improve ventilation, avoid outdoor exposures, wear dust mask, consider air purifiers if feasible
Call to action:
Engage with community efforts to improve air quality
Report increased cases to health department
Advocate for clean and renewable energy

Additional Resources
Maps:
Air quality data in the US: AirNow.gov (national forecast maps here, interactive map here, fire & smoke map here)
Worldwide AQI maps: here’s one from US consulates & embassies abroad and another one from Plume Labs, a start-up dedicated to making air quality information more accessible and comprehensive.
Datasets:
In the US: Air Quality Data Collected at Outdoor Monitors Across the US (EPA)
Around the world: Air pollution data portal (WHO)
Articles for further reading:
Air Cleaner Information for Consumers | California Air Resources Board
Example of a clinician writing an op-ed for climate action: A clean transportation system is the prescription my patients need (The Boston Globe)
Climate impacts of air pollution - Air quality and health (WHO)
Air pollution and climate change: two sides of the same coin (UN Environment Programme)
Synergistic health effects of air pollution, temperature, and pollen exposure: a systematic review of epidemiological evidence (academic article in Environmental Health)
Climate Changes Health: Respiratory Health (American Public Health Association/APHA)
Specifically for child health:
Climate change and air pollution impacts on children's health (Stanford Woods Institute for the Environment)
Wildfires and Children's Health - Western States PEHSU (UCSF)
Further Learning
Climate Resources for Health Education (CRHE) offers additional learning resources relevant to this case. Please explore the below links:
PBL case on OSS 1.3 Types of PM air pollution and cardiac morbidity and mortality
PBL case on OSS 2.3 Environmental Allergic Disease, Immunology, and Climate Change
PBL case on OSS 2.5 Global health: indoor biofuel combustion and lung disease
PBL case on OSS 3.2 Metabolic Disease: Type 2 diabetes and air pollution

References
A Systems Approach to Air Pollution – East Africa: Synthesis Report ASAP-East Africa Research Team February 2020
Achakulwisut P, Mickley LJ, Anenberg SC. Drought-sensitivity of fine dust in the US Southwest: Implications for air quality and public health under future climate change. Environ Res Lett. 2018;13(5):054025. doi:10.1088/1748-9326/aabf20
Aguilera R, Corringham T, Gershunov A, Benmarhnia T. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat Commun. 2021;12(1):1493. doi:10.1038/s41467-021-21708-0
Air pollution levels rising in many of the world’s poorest cities. World Health Organization. Published May 12, 2016. https://www.who.int/news/item/12-05-2016-air-pollution-levels-rising-in-many-of-the-world-s-poorest-cities
Air Quality Index (AQI) Basics. Airnow.gov. https://www.airnow.gov/aqi/aqi-basics/
Bard RL, Ijaz MK, Zhang J (Jim), Li Y, Bai C, Yang Y, et al.. Interventions to Reduce Personal Exposures to Air Pollution: A Primer for Health Care Providers. Global Heart. 2019;14(1):47–60. DOI: http://doi.org/10.1016/j.gheart.2019.02.001
Bartington, S.E., Kabera, T., Woolley, K.E., Avis, W., Pope, F.D., Thomas, G.N. (2020) Briefing Note: Household air pollution in households using charcoal fuel in Kigali, Rwanda Birmingham, UK: University of Birmingham
Batchelor S, Brown E, Leary J, Scott N, Alsop A, Leach M. Solar electric cooking in Africa: Where will the transition happen first? Energy Research & Social Science. 2018;40:257-272. doi:10.1016/j.erss.2018.01.019
Carlsten C, Salvi S, Wong GWK, et al. Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public. Eur Respir J 2020; 55: 1902056 [https://doi.org/10.1183/13993003.02056-2019]
Cepeda M, Schoufour J, Freak-Poli R, Koolhaas CM, Dhana K, Bramer WM, Franco OH. Levels of ambient air pollution according to mode of transport: a systematic review. Lancet Public Health. 2017 Jan;2(1):e23-e34. doi: 10.1016/S2468-2667(16)30021-4. Epub 2016 Nov 26. PMID: 29249477.
Christopher Carlsten, Sundeep Salvi, Gary W.K. Wong, Kian Fan Chung. Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public. European Respiratory Journal 2020 55: 1902056; DOI: 10.1183/13993003.02056-2019Lancet 2020; 396: 1223–49
Crooks JL, Licker R, Hollis AL, Ekwurzel B. The ozone climate penalty, NAAQS attainment, and health equity along the Colorado Front Range. J Expo Sci Environ Epidemiol. Published online September 10, 2021. doi:10.1038/s41370-021-00375-9.
Finnegan J. Survey finds more than 9 in 10 people say doctors are the most trusted professionals. Fierce Healthcare. Published May 21, 2019. https://www.fiercehealthcare.com/practices/survey-finds-over-9-10-people-say-doctors-are-most-trusted-professionals
Frederick E. What we don’t know about wildfire smoke is likely hurting us. Science. Published February 14, 2020. https://www.science.org/content/article/what-we-don-t-know-about-wildfire-smoke-likely-hurting-us
Hadley MB, Baumgartner J, Vedanthan R. Developing a Clinical Approach to Air Pollution and Cardiovascular Health. Circulation. 2018 Feb 13;137(7):725-742. doi: 10.1161/CIRCULATIONAHA.117.030377. PMID: 29440198; PMCID: PMC5950725.
Hajat A, Hsia C, O’Neill MS. Socioeconomic Disparities and Air Pollution Exposure: A Global Review. Curr Envir Health Rpt. 2015;2(4):440-450. doi:10.1007/s40572-015-0069-5
Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O, Samet JM, Vineis P, Forastiere F, Saldiva P, Yorifuji T, Loomis D. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014 Sep;122(9):906-11. doi: 10.1289/ehp/1408092. Epub 2014 Jun 6. Erratum in: Environ Health Perspect. 2014 Sep;122(9):A236. PMID: 24911630; PMCID: PMC4154221
Health Chapter. National Climate Assessment. US Global Change Research Group, 2014.
Hope P. What the Inflation Reduction Act Could Mean for Your Next Appliance Purchase. Consumer Reports. Published August 12, 2022. https://www.consumerreports.org/appliances/inflation-reduction-act-and-new-electric-appliance-rebates-a3460144904/
https://www.airnow.gov/sites/default/files/2021-06/prepare-for-fire-season_1.pdf
Importance of Methane. US Environmental Protection Agency. Published June 9, 2022. https://www.epa.gov/gmi/importance-methane
Jbaily A, Zhou X, Liu J, et al. Air pollution exposure disparities across US population and income groups. Nature. 2022;601(7892):228-233. doi:10.1038/s41586-021-04190-y
Ken Lee K, Bing R, Kiang J, et al. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob Health. 2020 Nov; 8(11): e1427–e1434. Published online 2020 Oct 15. doi: 10.1016/S2214-109X(20)30343-0
Lebel ED, Finnegan CJ, Ouyang Z, Jackson RB. Methane and NOx Emissions from Natural Gas Stoves, Cooktops, and Ovens in Residential Homes. Environ Sci Technol. 2022;56(4):2529-2539. doi:10.1021/acs.est.1c04707.
Manisalidis I, Stavropoulou E, Stavropoulos A and Bezirtzoglou E (2020) Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 8:14. doi: 10.3389/fpubh.2020.00014
Opotowsky AR, Vedanthan R, Mamlin JJ. A case report of cor pulmonale in a woman without exposure to tobacco smoke: an example of the risks of indoor wood burning. Medscape J Med. 2008;10(1):22. Published 2008 Jan 29.
Rentschler J, Leonova N. Air pollution kills – Evidence from a global analysis of exposure and poverty. World Bank. Published May 18, 2022. https://blogs.worldbank.org/developmenttalk/air-pollution-kills-evidence-global-analysis-exposure-and-poverty
Rice MB, Thurston GD, Balmes JR, Pinkerton KE. Climate change. A global threat to cardiopulmonary health. Am J Respir Crit Care Med. 2014;189(5):512-519. doi:10.1164/rccm.201310-1924PP
Salas RN. Environmental Racism and Climate Change - Missed Diagnoses. N Engl J Med. 2021 Aug 18. doi: 10.1056/NEJMp2109160. Epub ahead of print. PMID: 34407333.
Sedghy F, Varasteh AR, Sankian M, Moghadam M. Interaction Between Air Pollutants and Pollen Grains: The Role on the Rising Trend in Allergy. Rep Biochem Mol Biol. 2018 Apr;6(2):219-224. PMID: 29766006; PMCID: PMC5941124.
Sood A. Indoor fuel exposure and the lung in both developing and developed countries: an update. Clin Chest Med. 2012;33(4):649-665. doi:10.1016/j.ccm.2012.08.003
Stewart S, Wilkinson D, Hansen C, Vaghela V, Mvungi R, McMurray J, Sliwa K. Predominance of heart failure in the Heart of Soweto Study cohort: emerging challenges for urban African communities. Circulation. 2008 Dec 2;118(23):2360-7. doi: 10.1161/CIRCULATIONAHA.108.786244. Epub 2008 Nov 24. PMID: 19029467.
Thurston GD, Balmes JR, Garcia E, et al. Outdoor air pollution and new-onset airway disease: an official American Thoracic Society workshop report. Ann Am Thorac Soc 2020;17:387-398.
U.S. Global Change Research Program. Fourth National Climate Assessment. Chapter 13: Air Quality
WEO-2017 Special Report: Energy Access Outlook, International Energy Agency, 2017 (https://webstore.iea.org/weo-2017-special-report-energy-access-outlook)
WHO fact sheet: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health
WHO fact sheet: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health
Who is at risk from air pollution? Minnesota Pollution Control Agency. https://www.pca.state.mn.us/air/who-risk-air-pollution
Wu X, Nethery RC, Sabath MB, Braun D, Dominici F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Sci Adv. 2020;6(45):eabd4049. doi:10.1126/sciadv.abd4049